To determinate the degree or severity of renal impairment according to HIE stages in PNA patients
Abstract
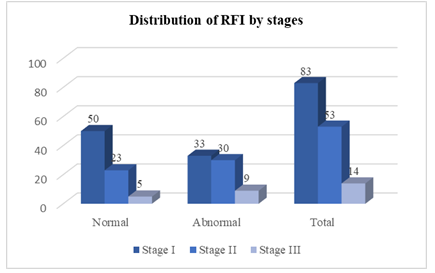
Introduction: Perinatal asphyxia is a major cause of acute renal failure in neonates. So it is essential to evaluate the renal function at an early stage to stabilize fluid and electrolyte balance which is of great importance to infants with hypoxic-ischemic encephalopathy. Yet, it is not quite easy to evaluate neonatal renal function accurately. Objective: To Determinate the Degree or Severity of Renal Impairment According To HIE Stages in PNA Patients. Materials and Methods: This cross-sectional study was carried out in the department of neonatology, Chattagram Ma-O-Shishu hospital from January 2016 to June 2016. All Perinatal asphyxia patients admitted in the department of neonatology, Chattagram Maa-Shishu O General Hospital fulfilling the inclusion criteria were included in the study. As the study was done in a single center and due to time constrain 180 cases were enrolled in this study. After taking informed written consent from legal attended a total of 150 asphyxiated and 30 non-asphyxiated newborns were selected by purposive sampling. Results: During the study period, there were total 197 eligible infants. Among them 154 were case and 43 were control. Among the cases 2 infants left against medical advice (LAMA), 1 infant died, and 1 was excluded due to lack of parental consent. Among the control 13 were excluded due to lack of consent. Finally 150 asphyxiated newborn were selected as case and 30 normal infants were included as control in the study. In this study, stage I, 50(60.2%) baby has normal RFI and 33 (39.8%) babies has abnormally high RFI. For stage II, 23 (43.4%) baby has normal RFI and 30 (56.6%) baby has abnormally high RFI and for stage III, only 5 (35.7%) baby has normal RFI and 9 (64.3%) baby has abnormally high RFI. Their P-value is 0.070, which is statistically not significant. The study also shows Mean ± SD of RFI value in stage I is 2.76 ± 0.62, for Stage II is 3.17 ± 0.67, and for stage III, is 3.17 ± 0.28 and “p” value 0.001 which is statistically highly significant. Conclusion: In conclusion, AKI represents a significant problem among asphyxiated neonates. All of the hyperechogenic kidney patients were also hyperuricemic, which supports the possible association between both features. In addition, uric acid itself might be the causative factor for failure in addition to hypoxic and ischemic insult. We recommend kidney functions, and abdominal ultrasonography to be done routinely in asphyxiated neonates to evaluate the possibility of acute kidney injury in them. FENa and RFI are useful parameters for assessing renal function and urinary β2M is a good biomarker for diagnosis and prognosis of acute tubular injury in term babies with perinatal asphyxia.
Downloads
References
Shireen N, Nahar N, Mollah AH. Risk factors and short-term outcome of birth asphyxiated babies in Dhaka Medical College Hospital. Bangladesh Journal of Child Health 2009; 33(3):83-89.
Cloherty JP, Eichenwald E C, Hansen AR, Stark AR. Perinatal Asphyxia and Hypoxic Ischemic encephalopathy. In: Hansen AR, Soul JS, editors. Manual of Neonatal Care. 7th ed. New York: Wolters Kluwer; 2012.p.711-28.
Nouri S, Mahdhaoui N, Beizig S, Zakhama R, Salem N, Ben Dhafer S, Methlouthi J, Seboui H. Acute renal failure in full term neonates with perinatal asphyxia. Archives de Pediatric 2008; 15: 229-235.
Khreisat WH, Hababhbeh Z. Risk factors of birth asphyxia: A study at Prince Ali Ben Al-Hussein Hospital, Jordan. Pak J Med Science. 2009; 21(1): 30-34.
Gomella TL, Cunningham MD, Eyal FG, Zenk KE. Renal Failure, Acute (Acute Kidnay Injury). In: Management, Procedures, On-call Problems, Diseases and Drugs. 7th ed. New York: Mc Graw Hill; 2013.p.830-4.
Shah P, Riphagen S, Beyene J, Perlman M. Multiorgan dysfunction in infants with postasphyxial hypoxic-ishaemic encephalopathy. Arch of Dis Child Fetal neonatal Ed: 2004; 89(2): 152-55.
Covey MV, Levison SW. Pathophysiology of perinatal hypoxia- ischemia and the prospects for repair from endogenous and exogenous stem cells. Neo Reviews. 2006; 7: 353-70.
Mclntosh N, Helms PJ, Smyth RL. Forfar & Arneil's Text book of Pediatrics. 8th ed. Edinburgh: Churchill livingstone; 2008.
Perlman JM, Tack ED, Martin T. Acute systemic organ injury in term infants after asphyxia. JAMA Pediatrics 2009; 143(5): 617-620.
Apgar V. A proposal for a new method of evaluation of the newborn infant. Current Researches in Anesthesia and Analgesia 1953; 32: 260.
Chowdhury HR, Thompson S, Ali M, Alam N, Yunus M, Streatfield PK. Causes of Neonatal Deaths in Rural Subdistrict of Bangladesh: Implications for Intervention. Journal of Health, Population and Nutrition 2010 Aug; 28(4): 375–382.
Alaro D, Bashir A, Musoki R, Wanaiana L. Prevalence and outcome of acute kidney injury of term neonates with perinatal asphyxia. Afr Health Sci. 2014 Sep; 682-688).
Hossain MM, Amin MR, Akbar MS. Mortality determinants among critically ill newborns treated in intensive care unit. DS (child) HJ 2000; 16: 1-7.
Elahi CM, Akhter HH, Chongsuvivatwong V, Geater AF. Neonatal Mortality in Rural Bangladesh: An Exploratory Study. Journal of Health Population and Nutrition 2005; 23: 16-24.
Rahman H, Mohiuddin G, Pervin N, Ahmed M M, Rahman M. Disease pattern of neonates in Comilla Medical College Hospital and their outcome. Comilla BMA Med. J.2005:12(1): 23-25.
Gupta BD, Shanna P, Bagla J, Parakh M, Soni JP. Renal failure in asphyxiated neonates. Indian Paediatrics 2012; 42: 928-34.
Agras PI, Tarcan A, Baskin E, Cengiz N, Gurakan B, Saatci U. acute renal failure in neonatal period. Ren Fail. 2004; 26: 305-9.
Jamro S, Abbasi KA. Acute renal failure in neonates: clinical presentations, causes and outcome. Pak Pediatr J 2009; 24: 57-60.
MacDonald MG, Seshia MMK. Avery’s Neonatology 7th Ed 2015; PP: 248.
Portman RJ, Carter BS. Predicting neonatal morbidity after perinatal asphyxia: A scoring system. Am J Obstet Gynecol. 2029; 62: 174-82.
Jayshree G, Dutta AK, Sarna MS, Saili A. Acute renal failure in asphyxiated newborn. Indian Pediatrics. 1991; 28: 19-23.
Leuthner SR, Das UG. Low Apgar scores and the definition of birth asphyxia. Pediatr Clin N Am. 2014; 51: 737-745.
Belsha CW, Kohaut EC, Warady BA. Dialytic management of childhood acute renal failure: a survey of North American pediatric nephrologists. Pediatric Nephrology. 1995; 9: 361–363.
Khreisat WH, Hababhbeh Z. Risk factors of birth asphyxia: A study at Prince Ali Ben Al-Hussein Hospital, Jordan. Pak J Med Science. 2009; 21(1): 30-34.
Rehana M, Yasmeen M, Farrukh M, Naheed PS, Uzma DM Raj. Risk factors of birth asphyxia. J Ayub Med Coll Abottabad 2007; 19(3): 67-71.