Incidence and Predictors of Nasopharyngeal Airway to Facilitate Nasotracheal Intubation
Abstract
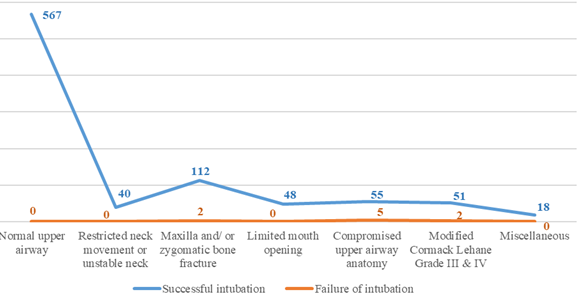
Background: Nasotracheal intubation is the most frequent approach of airway management in oral and maxillofacial surgical procedure. However, many times, it is related to ensuing bleeding from trauma to nasopharyngeal mucosa. This study was done to determine how effectively nasopharyngeal airways (NPAs) performed at making nasopharyngeal insertion simple and minimize trauma during nasotracheal intubation. Objectives: The aim of this study is to determine the incidence and predictors of nasopharyngeal airway to facilitate nasotracheal intubation. Methods: This study was carried out in the Anaesthesiology Department of Dhaka Dental College and Hospital. The subjects of the study were the patients who underwent maxillofacial surgery and required nasotracheal intubation. Nasotracheal intubation was done on 900 patients during the study period from January 2022 to December 2022. Results: The majority of patients 891(99.0%) had successful nasotracheal intubation. The patients in this study ranged in age from 10 to 60 years old and the majority were male 685(76.1%). A small percentage of patients reported postoperative complications such as runny nose 12 (1.3%), epistaxis or nasal bleeding 10(1.2%), nasal trauma or pain 12(1.3%), inflammation or ulceration of the nose with full recovery 6(0.6%), and sinusitis 10(1.2%) among individuals. For atraumatic nasotracheal intubation, nasal cavity dilatation with nasopharyngeal airways was useful. Conclusions: Dilatation of nasal cavity with nasopharyngeal airways (NPAs) extensively eases the insertion of endotracheal tube (ETT) into the nasopharynx and significantly decreases the incidence and severity of trauma and bleeding during nasotracheal intubation.
Downloads
References
Hall CE, Shutt LE. Nasotracheal intubation for head and neck surgery. Anaesthesia. 2003 Mar;58(3):249-56.
Elwood T, Stillions DM, Woo DW, Bradford HM, Ramamoorthy C. Nasotracheal intubation: a randomized trial of two methods. The Journal of the American Society of Anesthesiologists. 2002 Jan 1;96(1):51-3.
O’hanlon J, Harper KW. Epistaxis and nasotracheal intubation-prevention with vasoconstrictor spray. Irish journal of medical science. 1994 Jan;163(1):58-60.
El-Seify ZA, Khattab AM, Shaaban AA, Metwalli OS, Hassan HE, Ajjoub LF. Xylometazoline pretreatment reduces nasotracheal intubation-related epistaxis in paediatric dental surgery. British journal of anaesthesia. 2010 Oct 1;105(4):501-5.
Kay J, Bryan R, Hart HB, Minkel DT, Munshi C. Sequential dilation: a useful adjunct in reducing blood loss from nasotracheal intubation. Anesthesiology. 1985;63(3A):A259.
Kim YC, Lee SH, Noh GJ, Cho SY, Yeom JH, Shin WJ, Lee DH, Ryu JS, Park YS, Cha KJ, Lee SC. Thermosoftening treatment of the nasotracheal tube before intubation can reduce epistaxis and nasal damage. Anesthesia & Analgesia. 2000 Sep 1;91(3):698-701.
Seo KS, Kim JH, Yang SM, Kim HJ, Bahk JH, Yum KW. A new technique to reduce epistaxis and enhance navigability during nasotracheal intubation. Anesthesia & Analgesia. 2007 Nov 1;105(5):1420-4.
Prior S, Heaton J, Jatana KR, Rashid RG. Parker flex-tip and standard-tip endotracheal tubes: a comparison during nasotracheal intubation. Anesthesia progress. 2010;57(1):18- 24.
Yamamoto T, Flenner M, Schindler E. Complications associated with nasotracheal intubation and proposal of simple countermeasure. Anaesthesiology Intensive Therapy. 2019 Feb 6;51(1):75-7.
Chauhan V, Acharya G. Nasal intubation: a comprehensive review. Indian Journal of Critical Care Medicine: Peer-reviewed, Official Publication of Indian Society of Critical Care Medicine. 2016 Nov;20(11):662.
Coplans MP. A cuffed nasotracheal tube for microlaryngeal surgery. Anaesthesia 1976; 31: 430–2.
Keen RI, Kotak PK, Ramsden RT. Anaesthesia for microsurgery of the larynx. Annals of the Royal College of Surgeons of England 1982; 64: 111–13.
Sim WS, Chung IS, Chin JU, Park YS, Cha KJ, Lee SC, Kim YC. Risk factors for epistaxis during nasotracheal intubation. Anaesthesia and intensive care. 2002 Aug;30(4):449-52.
Adamson DN, Theisen FC, Barrett KC. Effect of mechanical dilation on nasotracheal intubation. Journal of oral and maxillofacial surgery. 1988 May 1;46(5):372-5.
Lewis JD. Facilitation of nasogastric and nasotracheal intubation with a nasopharyngeal airway. The American Journal of Emergency Medicine. 1986 Sep 1;4(5):426.
Kihara S, Komatsuzaki T, Brimacombe JR, Yaguchi Y, Taguchi N, Watanabe S. A silicone-based wire-reinforced tracheal tube with a hemispherical bevel reduces nasal morbidity for nasotracheal intubation. Anesthesia & Analgesia. 2003 Nov 1;97(5):1488-91.
Kameyama K, Watanabe S, Kano T, Kusukawa J. Effects of nasal application of an epinephrine and lidocaine mixture on the hemodynamics and nasal mucosa in oral and maxillofacial surgery. Journal of Oral and Maxillofacial Surgery. 2008 Nov 1;66(11):2226-32.
Sanuki T, Hirokane M, Kotani J. Epistaxis during nasotracheal intubation: a comparison of nostril sides. Journal of oral and maxillofacial surgery. 2010 Mar 1;68(3):618-21.
O’hanlon J, Harper KW. Epistaxis and nasotracheal intubation-prevention with vasoconstrictor spray. Irish journal of medical science. 1994 Jan;163(1):58-60.
Dhakate VR, Singam AP, Bharadwaj HS. Evaluation of nasopharyngeal airway to facilitate nasotracheal intubation. Annals of Maxillofacial Surgery. 2020 Jan;10(1):57.
Enk D, Palmes AM, Van Aken H, Westphal M. Nasotracheal intubation: a simple and effective technique to reduce nasopharyngeal trauma and tube contamination. Anesthesia & Analgesia. 2002 Nov 1;95(5):1432-6.
Morimoto Y, Sugimura M, Hirose Y, Taki K, Niwa H. Nasotracheal intubation under curve-tipped suction catheter guidance reduces epistaxis. Canadian Journal of Anesthesia. 2006 Mar;53(3):295-8.
Ahmed-Nusrath A, Tong JL, Smith JE. Pathways through the nose for nasal intubation: a comparison of three endotracheal tubes. British journal of anaesthesia. 2008 Feb 1;100(2):269-74.
Sugiyama K, Manabe Y, Kohjitani A. A styletted tracheal tube with a posterior-facing bevel reduces epistaxis during nasal intubation: a randomized trial. Canadian Journal of Anesthesia/Journal canadien d'anesthésie. 2014 May;61(5):417-22.